Abdominal pain is one of the most common symptoms that suggests a wide range of possible health problems, and one of the organs that often remains neglected in the first estimates is the pancreas. The pancreas, also known as pancreas, plays a key role in digestion and regulation of blood sugar. When there is a disturbance in its work, the pain that occurs can be specific, but also easily replaceable with pain caused by other organs such as the stomach, gall bladder or kidney.
Many wonder where the pancreas hurts, how to recognize that it is the source of the complaints and what are the symptoms that require medical help. The pain associated with the pancreas is often described as a deep, dull or stinging pain in the upper part of the abdomen, which can spread towards the back. Depending on the cause, the intensity and duration of the pain can vary – from mild discomfort to extremely strong and long-term pain that interferes with daily functioning.
In this article, we will explain exactly where the pancreas is located, how to recognize the pain associated with its diseases, which are the most common diseases of the pancreas, as well as when to worry and seek professional help. Proper understanding of symptoms is the key to timely diagnosis and treatment, especially in serious conditions such as acute pancreatitis or pancreatic cancer. It is also recommended to inform through expert sources such as Croatian Institute of Public Health.
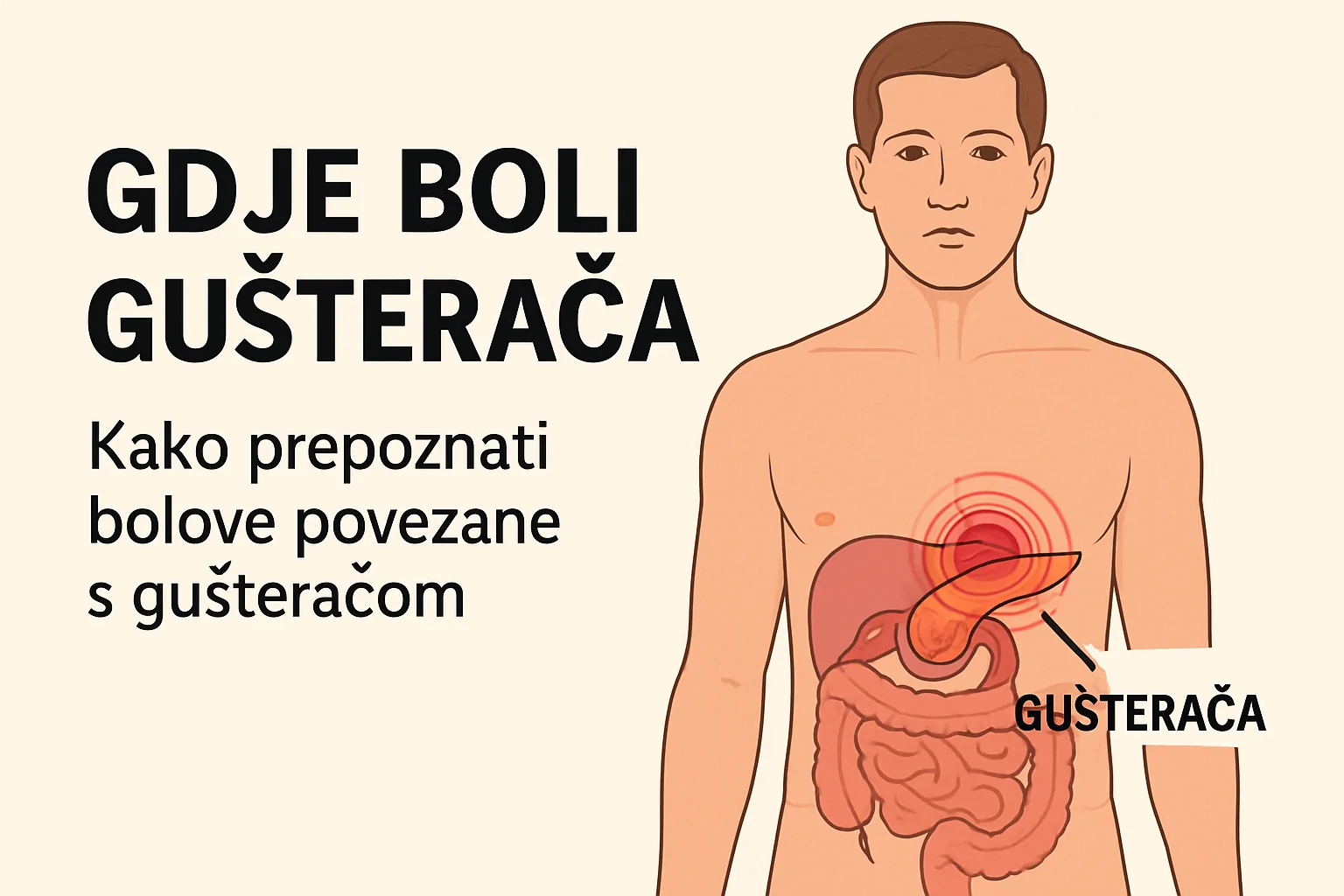
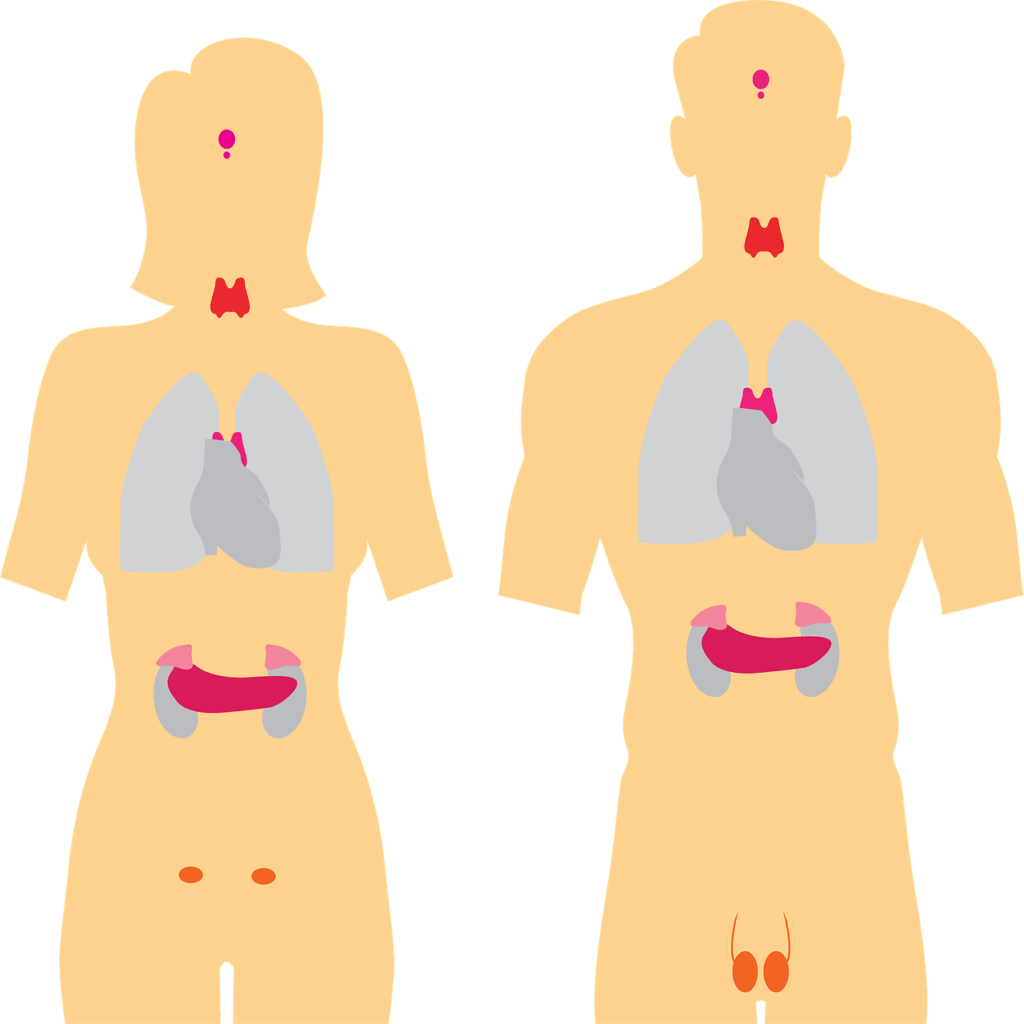
Where exactly is the pancreas in the body?
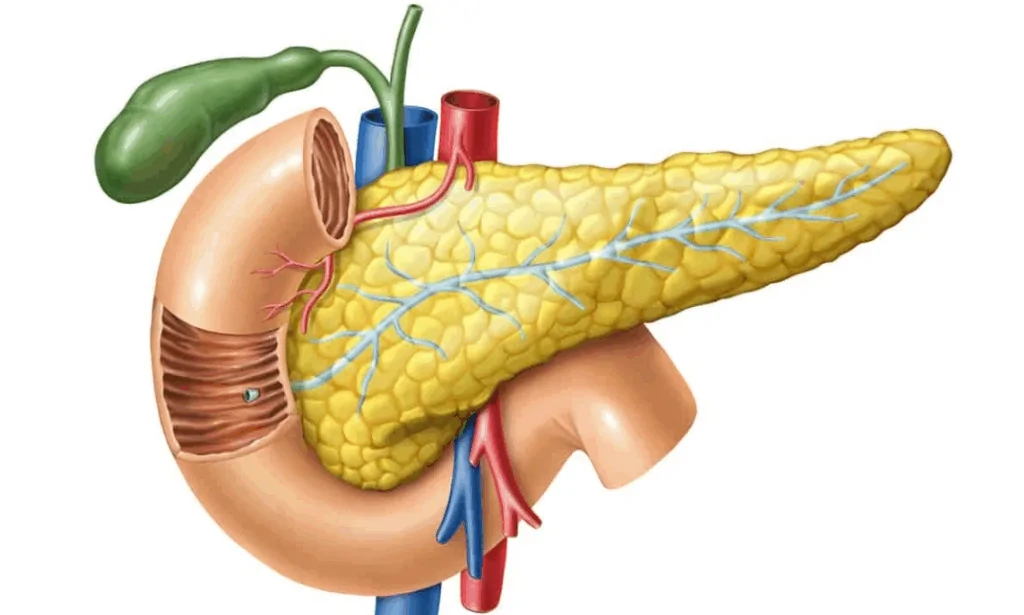
The pancreas is a vital organ located deep inside the abdominal cavity, just behind the stomach. It is located horizontally between the duodenum (the initial part of the small intestine) and the spleen, and extends across the upper part of the abdomen. Its length is approximately 15 to 20 centimeters, and it is divided into three main parts: head, body and tail.
- Pancreatic head It is located in the right part of the abdomen, inside the bend of the duodenum.
- pancreatic body It extends towards the middle of the upper part of the abdomen.
- The tail of the pancreas It is located in the left upper part of the abdomen, near the spleen.
Due to its location deep in the abdominal cavity, the pain associated with the pancreas may not always be easily recognizable. People often report pain that occurs in the middle part of the abdomen, just below the sternum, and the pain can also spread to the back, especially in case of more serious inflammation.
This deep and central location is the reason why pain associated with the pancreas is often confused with problems of the stomach, bile or spine. Proper recognition of the anatomical position of the pancreas is the first step in understanding possible symptoms and timely diagnosing its diseases.
How to recognize pancreatic pain
Pain caused by the pancreas can be very specific, but also vary depending on the type and severity of the condition. The most common causes of pain associated with the pancreas include acute pancreatitis, chronic pancreatitis thee pancreatic tumors, and all of them can cause pain that differs in intensity, duration and localization.
The most common pain characteristics associated with the pancreas include:
- localization of pain: Pain most often occurs in the upper part of the abdomen, more precisely in the epigastric area (the area under the sternum), and often spreads towards the back.
- the nature of pain: It is described as a dull, constant, burning or stabbing pain. It can be mild and tolerable, but also very strong, especially with acute pancreatitis.
- aggravation of pain after eating: Food, especially fatty and heavy, can worsen symptoms because it stimulates the pancreas to work, which further irritates the inflamed tissue.
- Release of pain: Lying on your side with your knees drawn towards your chest sometimes brings relief, while lying on your back can make symptoms worse.
- accompanying symptoms: In addition to pain, nausea, vomiting, fever, bloating, diarrhea, loss of appetite and jaundice (yellowing of the skin and sclera) may occur.
In chronic pancreatic diseases, the pain can be permanent and exhausting, often accompanied by loss of body mass due to problems with digestion and absorption of nutrients.
It is important to emphasize that pancreatic pain can be mistaken for other abdominal organs, so it is crucial to pay attention to the overall clinical context and other symptoms that accompany them. In case of severe and sudden pain that does not go away, it is necessary to seek medical help immediately because it can be acute pancreatitis or other emergency. For additional information on symptoms and causes in English, see the article Mayo Clinic on Pancreatitis.
Difference between acute and chronic pancreatitis
Pancreatitis is an inflammation of the pancreas that can have different forms and causes, and is most often divided into acute and chronic pancreatitis. Although both forms affect the same organ, they differ in the duration, severity of symptoms, causes and consequences that leave the function of the pancreas.
acute pancreatitis
Acute pancreatitis is sudden inflammation of the pancreas which develops quickly and often requires urgent medical intervention. The most common causes are gallstones and excessive alcohol consumption, but it can also be triggered by certain medications, infections, trauma, high blood fat levels or autoimmune disorders.
Main features:
- Severe and severe pain in the upper abdomen, often spreading towards the back
- Nausea, vomiting, flatulence
- elevated body temperature
- Elevated pancreatic enzymes (amylase, lipase) in the blood
- In severe cases: organ damage, shock, and even fatal outcome
Most patients with acute pancreatitis recover with adequate hospital care, but recurring episodes can lead to chronic changes.
chronic pancreatitis
Chronic pancreatitis is Long-lasting and progressive inflammation of the pancreas which over time causes permanent damage and loss of function. It is most often associated with long-term alcohol consumption, but the causes can also be genetic, autoimmune, metabolic or idiopathic (unknown).
Main features:
- Long-term or occasional upper abdomen pain
- Digestive disorders (diarrhea, greasy stool, weight loss)
- decreased food digestion enzyme production
- Possible development of diabetes due to damage to the endocrine part of the pancreas
- The pancreas becomes scar tissue over time and loses function
Unlike the acute form, the symptoms of chronic pancreatitis develop slowly and gradually, and the treatment is long-term, often involving lifestyle changes, enzymatic replacements and pain control.
When pancreatic pain requires immediate medical attention
Although abdominal pain can be caused by many harmless conditions, pain associated with the pancreas may indicate a serious health problem that requires rapid medical evaluation and treatment. Timely reaction is essential to preventing complications that can be life-threatening, especially with acute pancreatitis.
Emergency medical attention should be sought in the following situations:
- Sudden and severe pain in the upper abdomen which does not pass and/or worsens with time
- Pain that radiates to the back, especially if it occurs in seizures and is accompanied by a feeling of pressure or tightness
- elevated body temperature, chills and rapid pulse, which may indicate infection or inflammation
- nausea and vomiting which do not stop, especially if dehydration occurs
- Jaundice – the appearance of yellow skin and eye color, which may mean blockage of the bile ducts
- A sudden drop in blood pressure, weakness, dizziness or loss of consciousness – which can signal a serious complication such as sepsis or internal bleeding
- touch belly sensitivity and tension of the abdominal muscles
In all these cases, it is not recommended to wait at home or take painkillers independently without consulting a doctor. The pancreas is a sensitive organ, and the complications of its inflammation can quickly escalate – including tissue necrosis, infections, damage to other organs and the development of diabetes.
If you have an earlier diagnosis of pancreatitis or problems with the pancreas, and the symptoms worsen or change, and this is the reason for immediate control. Timely diagnosis and treatment can significantly improve outcome and prevent permanent damage.
Diagnostics and treatment of pancreatic diseases
Since the symptoms of the pancreas disease often resemble the problems of other organs of the digestive system, precise diagnostic is key to making an accurate diagnosis and planning treatment. Modern medicine offers a number of methods that can detect inflammation, tumors, cysts or functional disorders of the pancreas.
Diagnostic methods:
-
Laboratory blood tests
- elevated levels amylase and lipase (pancreatic enzyme) indicate acute inflammation.
- Analysis of sugar, liver enzymes, fats and markers of inflammation additionally helps in assessing the condition.
-
Abdominal ultrasound
- Basic and often the first test to assess the structure of the pancreas and the presence of gallstones, cysts or enlarged ducts.
-
CT (computed tomography)
- A detailed scan of the pancreas that helps to identify complications of pancreatitis, tumors and organ damage.
-
MRCP or MRI of the abdomen
- Magnetic resonance imaging is used to display bile and pancreatic ducts without the need for invasive surgery.
-
Endoscopic ultrasound (EUS)
- A combination of endoscopy and ultrasound that provides a detailed insight into the interior of the pancreas, especially when tumors are suspected.
-
ERCP (endoscopic retrograde cholangiopancreatography)
- The diagnostic-therapeutic method used to remove gallstones or place a stent in the pancreatic ducts.
Treatment of pancreatic diseases:
Treatment depends on the type and severity of the disease and the general health condition of the patient.
-
acute pancreatitis:
- Hospital treatment, fluid replacement, pain control, occasional fasting, antibiotic therapy if there is an infection.
- Removal of the cause (eg gallstone surgery) after stabilizing the condition.
-
chronic pancreatitis:
- Long-term therapy: enzymatic substitutes for digestion, painkillers, nutritional support and blood sugar control.
- Avoiding alcohol and fatty foods is a must. Sometimes surgical procedures are required.
-
Pancreatic tumors:
- Depending on the stage and type, treatment may include surgical removal of the tumor, chemotherapy, radiation or palliative care.
- Early diagnosis significantly increases the chances of survival.
Regular controls, lifestyle changes and cooperation with the doctor are key factors in the treatment of pancreatic diseases and the preservation of its function. You can find more about diagnostic and treatment procedures on the website KBC Zagreb – Gastroenterology.