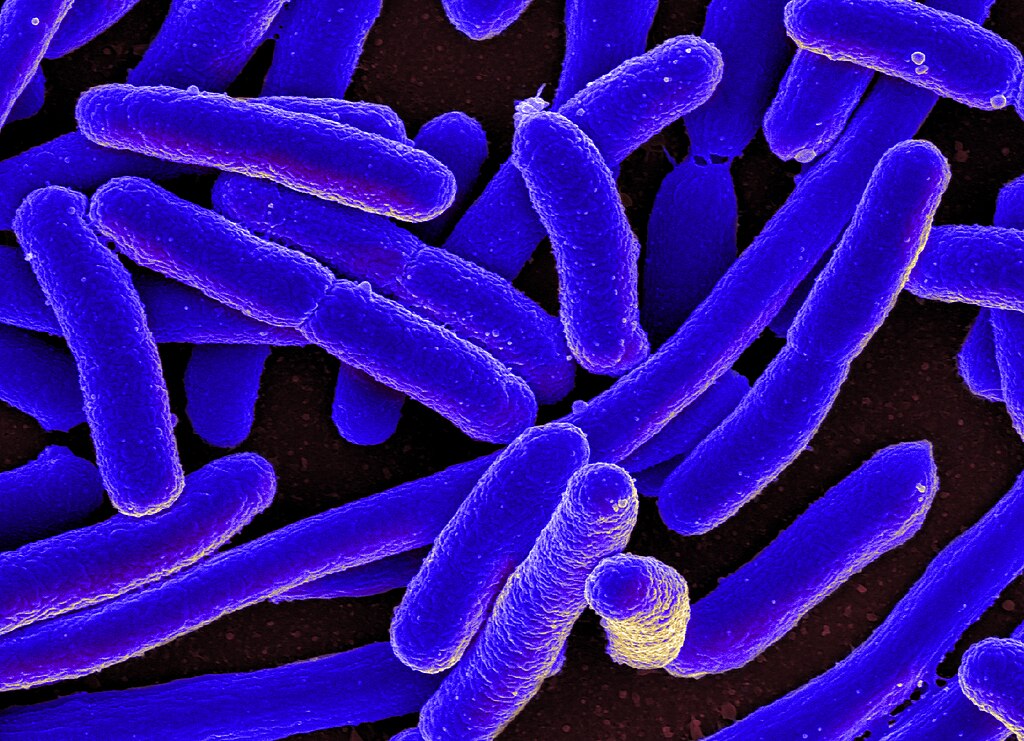
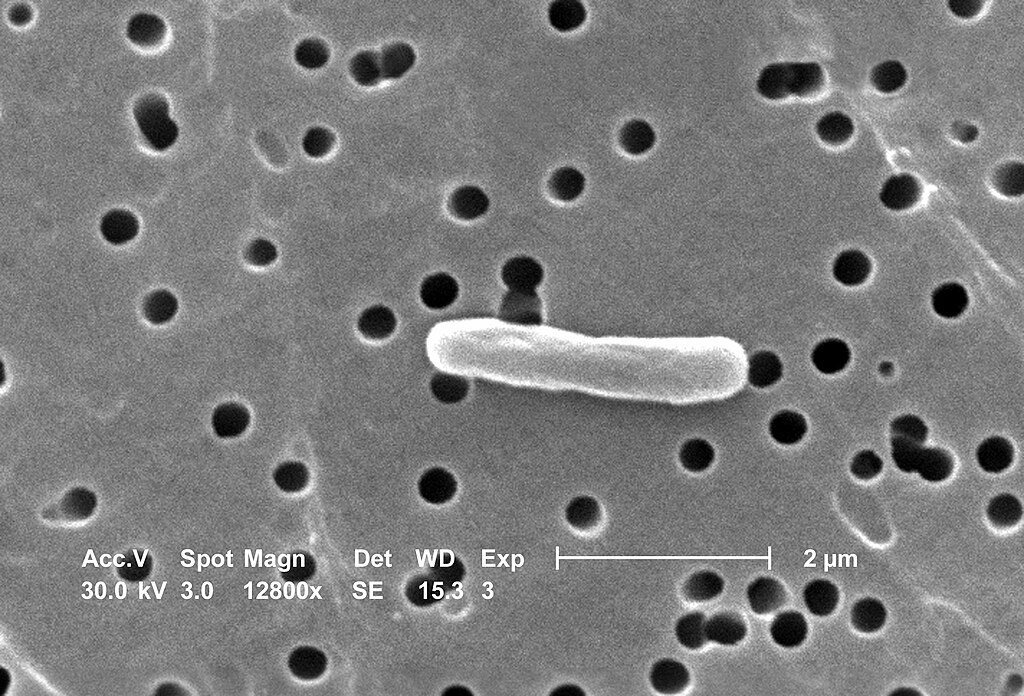
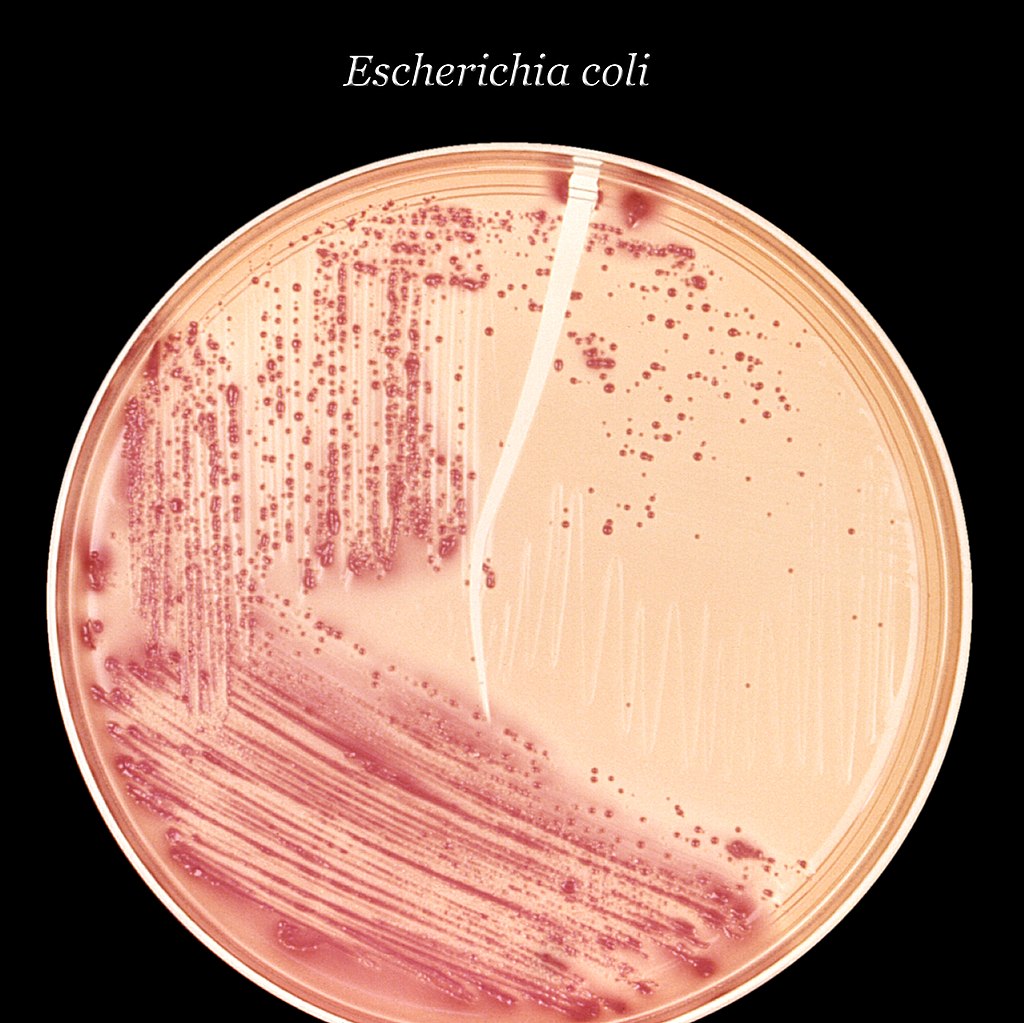
Bacteria in the urine mean that microorganisms are found in the urine – sometimes they really cause an infection (symptoms), and sometimes they are found accidentally without symptoms (asymptomatic bacteriuria). The most common cause of clinically significant urinary infections Escherichia coli (E. coli), which causes a large number of cases, especially in women.
The most common pathways of bacteria
- Bacteria from the intestine (eg E. coli) migrate towards the urethra and bladder (a common reason in women).
- Catheters or instrumental tests of the urinary system.
- Sometimes bacteria come from blood (less often) or food/environment (in specific situations).
which are typical Symptoms of urinary infection? (bacteria in urine symptoms)
The most common symptoms of a lower urinary tract infection (cystitis) are:
- burning when urinating (dysuria), pain and discomfort when urinating;
- frequent, incomplete urination;
- cloudy, dark or bloody urine;
- unpleasant smell of urine;
- Pressure or pain in the lower abdomen (via the bladder).
Read our post: An old remedy for itchy skin – natural solutions that work
If the infection spreads to the kidneys (pyelonephritis), the following may occur: fever, chills, severe back/side pain, nausea and vomiting – then an urgent medical assessment is required.
How is ‘bacteria in the urine’ diagnosed?
- Quick urine test (urinalysis) – Detects white blood cells, nitrites and blood.
- Urine culture (bacteria will kill?) – confirms which bacteria cause infection and which antibiotics are sensitive. It is recommended before or after the start of antibiotic therapy, depending on the clinical situation.
- The doctor will assess the symptoms, risk (men, pregnant women, diabetics, chronic patients) and decide on therapy. (Details on diagnostics are available in primary care guidelines.)
Treatment: best remedy for urinary infections (antibiotics and therapeutic approach)
- antibiotics are the standard and most common therapy for symptomatic bacterial urinary infections. The choice of drug depends on the location of the infection (spike vs. kidneys), severity of symptoms, allergies and local resistance data. In practice, drugs such as nitrofurantoin, trimethoprima-sulfamethoxazole or cephalosporin; In more complex infections, other options are applied. The doctor usually prescribes a short course (eg 3 days for uncomplicated cystitis in women), and a longer course for complications or men.
- Men and urinary infections: Infections in men are less common, but more often they are considered ‘complicated’ and require more thorough treatment (ultrasound, culture, longer therapy). Medical assessment is key.
Read our post: How to reduce cholesterol in 26 days naturally safe and easy
Example: What does therapy for common bladder infections look like (uncomplicated cystitis)
- Women without complications: a short course of antibiotics (eg nitrofurantoin for 5 days or trimethoprim-sulfamethoxazole for 3 days – according to the doctor’s assessment).
- Men: often longer therapy and further diagnostics.
Always finish the prescribed course of antibiotics and return to the doctor if the symptoms do not go away or worsen.
Over-the-counter medications and medications to relieve symptoms (non-prescription urinary infections)
- Phenazopyridine (Phenazopyridine) – Available in some countries as a remedy for relieving pain and burning when urinating. It acts as an analgesic that ‘an anesthetize’ urinary tract, but It does not cure infection – Only temporarily relieves symptoms. It is used for a short time and with caution (it does not change the color of urine to orange/red) and is not a substitute for an antibiotic if necessary.
- Other OTC preparations (pain/antipyretics, increased fluid intake, thermal compresses) can help while therapy lasts.
WARNING: Some countries limit or withdraw phenazopyridine for regulatory reasons – consult a local pharmacist or doctor before taking it.

Natural remedies and prevention: what really works? (burning when urinating natural remedy, bacteria in the urine natural treatment)
- Cranberry / Cranberry: Evidence shows that certain Cranberry products (juice, concentrates) may reduce the frequency of recurrent infections in some women. A Cochrane review indicates a moderate reduction in the risk of re-infection. However, Cranberry it is not a medicine For the current infection – it is more of a preventive measure.
- hygiene and habits: Front-to-back wiping, urination after intercourse, enough fluids and adequate personal hygiene reduces the risk. Antibiotic resistance is a real problem – therefore prevention is important.
- Probiotics and nutrition: Some data suggest the possible benefit of local lactobacilator preparations in women with recurrent UTIs, but the evidence is not unique.
Complications and “dangerous bacteria in the urine”
- If the infection spreads and affects the kidney, the risk of sepsis and permanent kidney damage increases. Emergency medical assistance is required at high temperature, severe pain, nausea/vomiting or signs of systemic infection.
- Antibiotic resistance: Some bacteria become resistant to common antibiotics, which is why the doctor often asks for a culture and antibiogram to adapt the therapy.

Short practical tips (which you can do immediately)
- If you have mild symptoms: drink enough fluids, avoid irritants (coffee, alcohol), you can take an OTC analgesic, but contact your doctor if symptoms last >48–72 hours.
- If you have a high fever, severe pain in the hip/back, nausea/vomiting or a significant trace of blood in the urine — seek immediate medical attention.
Conclusion and call to action
Bacteria in urine (bacteria in urine) They often cause unpleasant, but treatment has a good chance when properly diagnosed and treated. If you have symptoms such as burning when urinating, frequent urination or fever, talk to your doctor to do a urine test and if necessary, get the appropriate medicine. If you often have recurrent urinary infections, talk to your doctor about preventive measures (eg evaluation, possible prophylaxis, changes in habits, the possibility of a cranberry preparation).
Cover photo: Lehmann R., CC BY 4.0, Via Wikimedia Commons
